हिंदी में पढ़ने के लिए मेनू बार से हिंदी भाषा चयन करें।
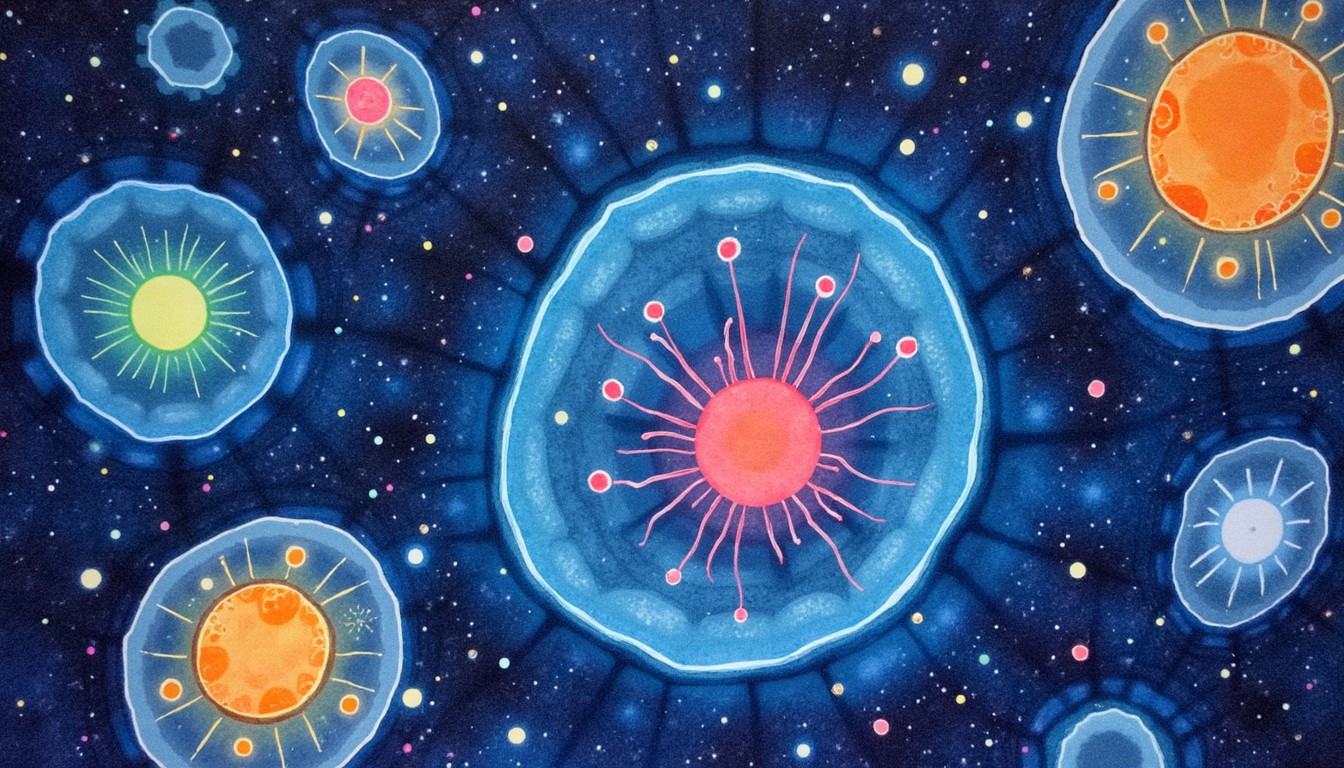
🌱 What Are iPS Cells?
iPS cells or induced pluripotent stem cells are a type of stem cell that scientists can create from ordinary adult cells — like skin or blood cells — and reprogram them to behave like embryonic stem cells.
These cells have the ability to become any type of cell in the body — such as heart cells, nerve cells, liver cells, or even brain cells. In short, they are man-made master cells that hold the power to rebuild damaged tissues or even entire organs.
How Were iPS Cells Discovered?

The concept of iPS cells was introduced in 2006 by Japanese scientist Dr. Shinya Yamanaka. He found that by inserting just four specific genes into adult mouse cells, those cells could be “reprogrammed” back to an embryonic-like state.
In 2007, the same method was successfully applied to human cells. For this groundbreaking work, Dr. Yamanaka was awarded the Nobel Prize in Physiology or Medicine in 2012.
🧪 How Are iPS Cells Made?
The process of creating iPS cells involves:
- Collecting adult cells from a person (like skin cells)
- Introducing specific genes using safe viruses or gene-editing tools like CRISPR
- The adult cells start to revert into a primitive, pluripotent state
- These cells are now capable of turning into any cell type under the right conditions
This technique is revolutionary because it does not require human embryos, solving many ethical concerns tied to traditional embryonic stem cell research.
What Are iPS Cells Used For?
iPS cells are already being used in lab research and clinical trials for several medical conditions. Some of their major uses include:
- Disease Modeling: Scientists grow diseased cells in labs to better understand conditions like Alzheimer’s, Parkinson’s, or heart disease.
- Drug Testing: Pharma companies test new drugs on lab-grown cells to check effectiveness and side effects.
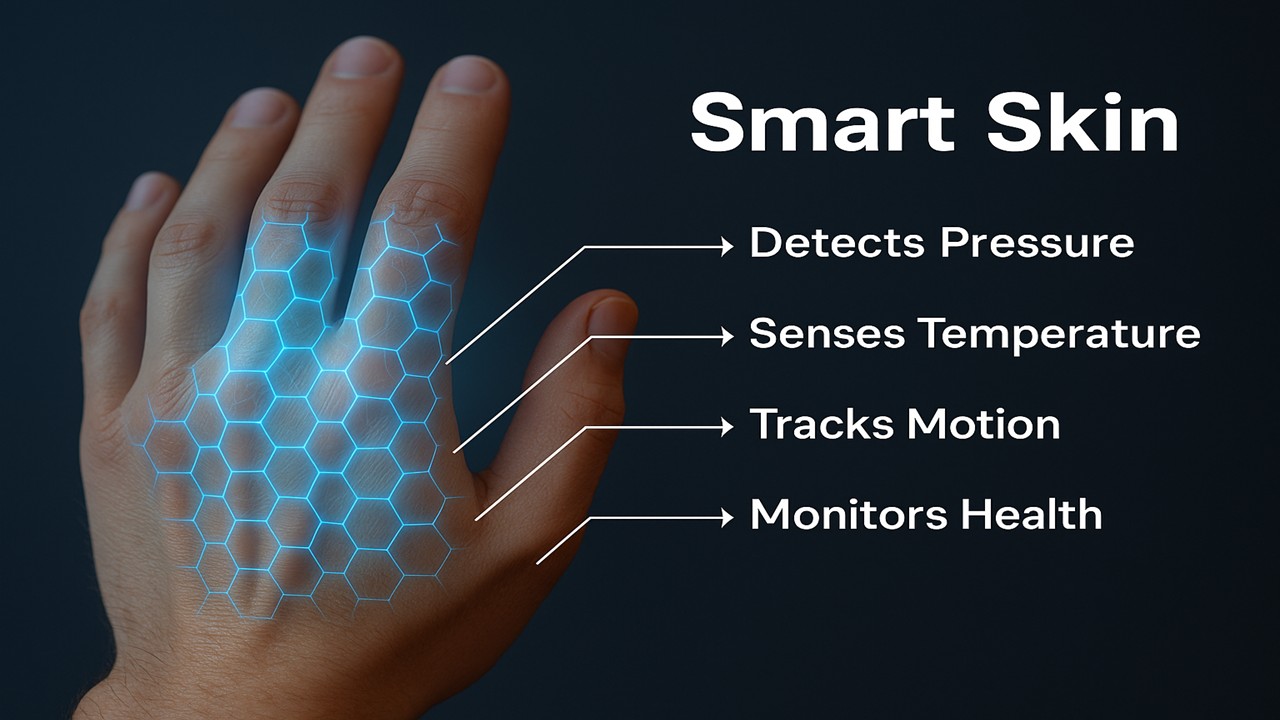
- Tissue Repair: Efforts are ongoing to use iPS cells to regrow retinal cells, skin, cartilage, and even heart muscle.
- Personalized Medicine: Since iPS cells can be made from the patient’s own body, they reduce rejection risks in future treatments.
🌍 Which Countries Are Leading in iPS Cell Research?
Several countries are investing in iPS research, with Japan leading the way.
- 🇯🇵 Japan – Home of the pioneer Dr. Yamanaka and Kyoto University’s iPS Cell Research Center
- 🇺🇸 USA – Harvard, Stanford, and NIH are deeply involved in clinical trials
- 🇩🇪 Germany – Advanced work in reprogramming and bioethics
- 🇮🇳 India – Early-stage research by AIIMS, NCBS, and IITs
What Are the Challenges?
While iPS cells are full of potential, they do come with challenges:
- Tumor Risk: If not controlled properly, these cells may cause cancer-like growth
- Genetic Mutations: Gene editing must be precise to avoid long-term risks
- Scalability: Producing high-quality iPS cells in large numbers is still complex
- Cost: The process is still expensive and needs refinement for mainstream use
Future Possibilities with iPS Cells
The future of iPS cells is incredibly bright:
- Patient-specific organ creation for transplants
- Gene-corrected cells for rare inherited diseases
- Artificial embryos for drug testing and reproductive research
- Full-body tissue engineering in regenerative labs
With AI, CRISPR, and 3D bioprinting all evolving alongside, iPS cells could power the next revolution in personalized medicine.
“iPS cells are one of the most powerful tools in modern medicine.
They are proof that science can reverse time — turning skin cells back into life-giving stem cells.
They give us the power to understand disease, to test drugs safely, and maybe one day, to grow entire organs in the lab.
The future of healing is not just treating illness… it’s about rebuilding health from your own cells.”